From her office overlooking the breathtaking coastline of Streaky Bay, Dr. Victoria Bradley once joked about having the most beautiful doctor’s practice in Australia. With farmland stretching to rocky shores and dolphins frolicking in the bay, the idyllic town is home to just 3,000 people, a few shops, and a tiny hospital.
But for Dr. Bradley, the town’s sole, permanent doctor, life was anything but idyllic. She spent years on call 24/7, managing both the local hospital and the general practitioner clinic. Running back and forth between patient rounds and appointments left little time for breaks, and on bad days, a hospital emergency would disrupt her already packed schedule.
Despite her dedication, the relentless pace eventually led to burnout. Two years ago, Dr. Bradley quit, and with her departure, the fragile healthcare system in Streaky Bay began to unravel. The town, once held together by the tireless work of its lone doctor, now faces the broader crisis of Australia’s crumbling universal healthcare system. With healthcare resources stretched thin across the country, Streaky Bay’s struggle is emblematic of a growing issue: Can Australia’s universal healthcare system be saved before more communities fall through the cracks?

Streaky Bay has become a symbol of a much broader national crisis. Across Australia, chronic underfunding is deepening a shortage of essential healthcare workers like Dr. Bradley. General practitioners are scarce, hospital staff are stretched thin, and specialists are increasingly hard to access. As public resources falter, wait times are soaring, fees are rising, and patients are bearing the brunt. In many cases, doctors are setting their own fees to stay afloat—leaving more Australians unable to afford basic medical care.
A healthcare system once hailed as one of the world’s best is now fraying under pressure. In many regions, it survives only because of the dedication of overstretched doctors and the resilience of local communities. But the cracks are widening, and the consequences are serious: more and more Australians are postponing, or skipping altogether, the care they need.
As the country prepares for its federal election on 3 May, healthcare has emerged as a key concern for voters. Both major parties are pledging billions in new funding. Yet health policy experts argue that these promises amount to temporary relief, not long-term reform. The real issue, they say, lies in how Australia’s healthcare system is structured and funded—a problem that requires bold political action, not just short-term fixes.
Australians are now asking a fundamental question: Is universal healthcare still a national priority? As communities like Streaky Bay struggle to stay afloat, the answer may determine the future of care across the country.
The cracks in a ‘national treasure’
For Renee Elliott, the fragility of Australia’s universal healthcare system became painfully clear when she was diagnosed with breast cancer—twice. Moving to Streaky Bay had been a lifestyle choice, not a healthcare risk. But when the 40-year-old discovered a cancerous lump in 2019, and then another four years later, the town’s lack of specialised medical services turned her battle into a logistical and financial nightmare.
With advanced care only available in Adelaide, more than 500km away, Renee was forced to make repeated long-distance trips—spending countless hours on the road and tens of thousands of dollars on travel, accommodation, and treatment. All this, while raising three children and running a small business. Government subsidies eventually covered some of the costs, but the initial burden was overwhelming.
“You’re trying to get better… but having to juggle all that as well. It was very tricky,” she reflects.
Her story reflects a deeper reality for many Australians: geography and postcode are increasingly shaping access to quality care. Even in a country that prides itself on universal healthcare, the promise of equal access feels increasingly out of reach for those in regional and rural areas. What was once a “national treasure” is now revealing its cracks—not just in budgets and policies, but in the lives of real people trying to navigate illness in a system that no longer guarantees support.

Australia’s modern healthcare system, launched four decades ago, was built on a powerful promise: that quality medical care would be a basic right, not a privilege. At its heart was Medicare—a public insurance scheme designed to make healthcare affordable and accessible to all Australians, regardless of income or geography.
The system worked simply in theory. Healthcare funding was a shared responsibility between state and federal governments. Patients could visit a doctor or hospital, flash their bright green Medicare card, and walk away with little to no out-of-pocket cost. The federal government would reimburse providers directly through tax-funded rebates. This allowed for “bulk billing,” where doctors accepted the Medicare rebate as full payment, offering care completely free at the point of service.
It was a system that tried to blend the universality of the UK’s National Health Service with the flexibility and innovation of the U.S. model. Medicare quickly became a beloved institution—a symbol of fairness and equality.
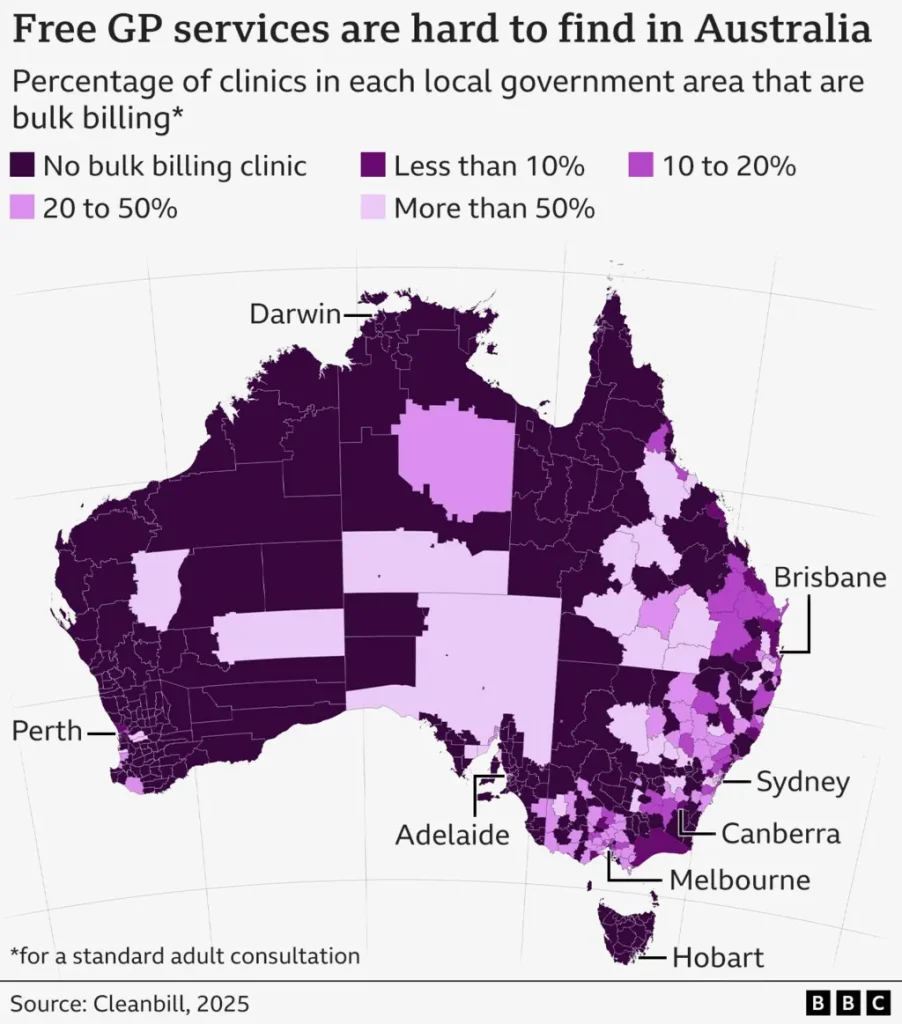
But today, many experts warn that the vision is unraveling. Bulk billing rates are falling. Public hospitals are overwhelmed. Private services, once a complementary option, now feel essential for timely care—if you can afford them. The once-balanced dual model is tipping into dysfunction.
As rising costs, staffing shortages, and inconsistent funding plague the system, Australia risks losing the very ideals that made Medicare a national treasure. Instead of combining the best of both worlds, some fear the country is heading toward a healthcare model with the worst of each.
There’s no question that Australia’s healthcare system still outperforms much of the world—especially in emergency response and acute hospital care. But the heart of the current crisis, and the political battleground of the upcoming election, lies elsewhere: in general practitioner (GP) services and primary care.
Traditionally dominated by private clinics, Australia’s primary care sector once operated smoothly under Medicare, with most GPs accepting government rebates as full payment. However, this model is buckling. Doctors argue that rebates have failed to keep pace with rising operational costs, making bulk billing increasingly unsustainable. At the same time, staffing shortages—despite efforts to attract international talent—are intensifying the pressure, driving prices up and access down.
Official statistics show that about 30% of Australians now pay a “gap fee” for a standard GP visit, averaging A$40 out of pocket. But health experts believe the real number is far higher. Seniors and children, who often qualify for fully bulk-billed visits, skew the data. And there’s an invisible population growing: people who avoid care altogether because they simply can’t afford it.
Brisbane electrician Callum Bailey is one of them. “Mum or my partner will pester and pester and pester… [but] I’m such a big ‘I’ll just suffer in silence’ person because it’s very expensive,” he admits. For 25-year-old Callum, the cost of living has already become overwhelming. “At my age, I probably should be in my prime looking for housing… [but] even grocery shopping is nuts. [I] just can’t keep up.”
His story echoes across the country—a quiet crisis unfolding in doctor’s waiting rooms, or rather, in the growing number of homes where people are simply not going at all.